Krista Riemer had already handled five or six life-threatening emergencies by the time Billy’s Gourmet Hot Dogs crossed her mind.
“It's all about the hot dog today,” she said. “Hot dogs and cheese fries.”
It’s one of her lunch-break favorites — if only she could find time for a break. On many days, mealtime never comes for Denver Health paramedics like Riemer and her two crewmates. The only sure thing is that the day will be chaotic. Riemer prefers it that way.
“It’s the greatest show on Earth,” she said. “We’re going to be outside and we get to run calls and we get to meet a hundred different people. Sometimes we get hot dogs.”
It’s all part of the job she’s been doing for the last 16 years. She loves the hustle. She’s good at it. And the city has perhaps never needed her more. It’s not just a growing population. Denver’s ambulances have become the last resort for people who fall through gaps in its safety net.
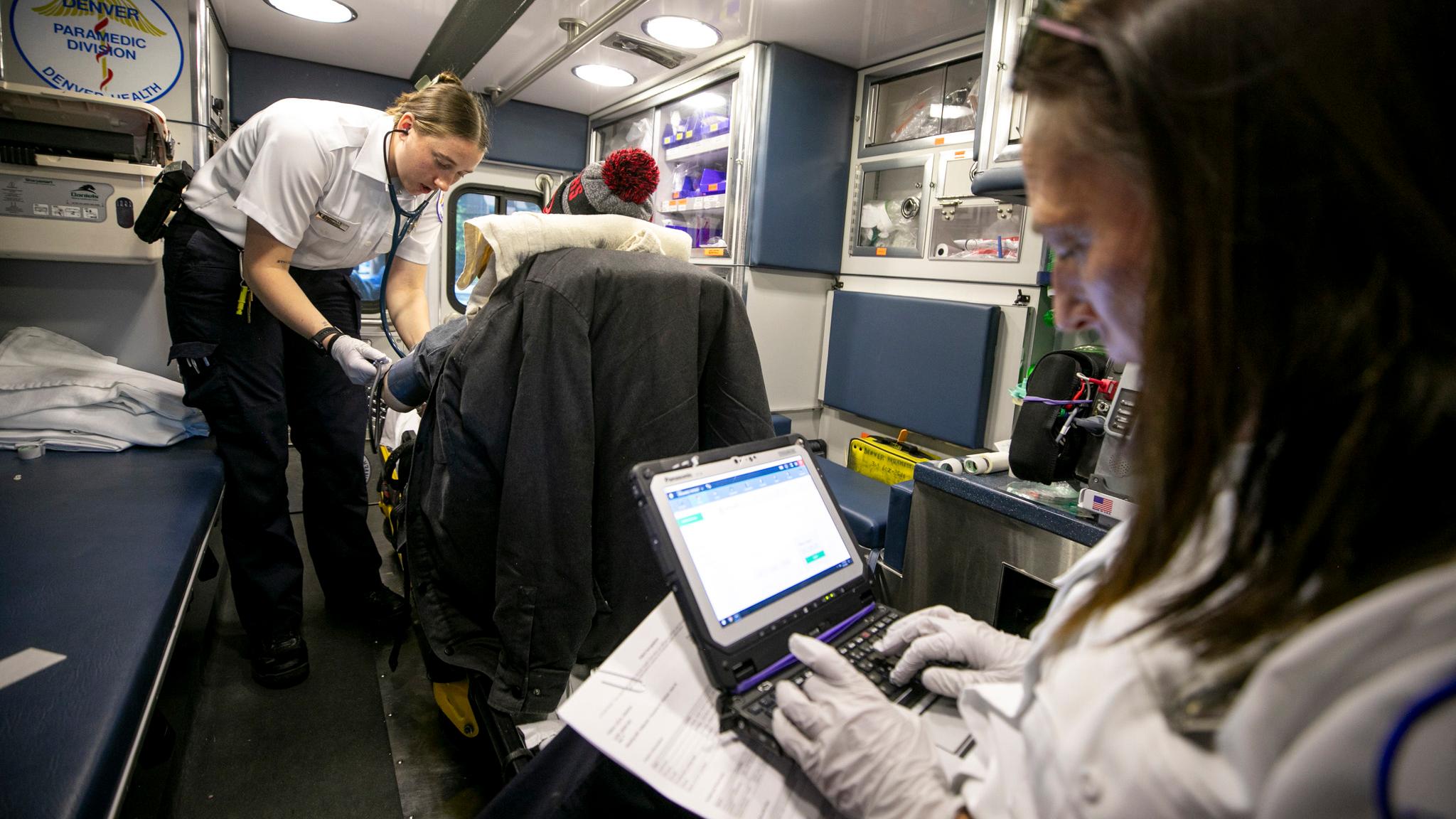
Denverite rode with Riemer as she made her rounds, sharing tips and stories with Brittan Ingalls, her latest trainee, and William Fish, who recently graduated from her tutelage. We wanted to see the hustle that underpins this essential city service.

Rationing resources in a world of need
Denverite joined the crew on an April afternoon as they finished a routine transport, taking a patient from a City Park West cancer center to a nearby emergency room. They thought this might be a moment for hot dogs — but then new marching orders crackled through their radios. Lunch would wait.
Someone had called 911 about a man passed out on a Colfax Avenue sidewalk. When the trio arrived, it was clear there was no emergency; he was asleep. Ingalls said this happens, and it’s obviously not ideal. She doesn’t want to discourage anybody from calling 911, but calls like this could keep paramedics from a real emergency.

Riemer, Ingalls and Fish helped the man back into his wheelchair. He didn’t need, or want, to go to the emergency room, but they could still help him. Thick bandages wrapped around his feet needed changing, so they crouched on the ground beneath him to apply a fresh set. Some of his toes were missing, others black, apparently lost to frostbite.
“He just had surgery on his feet, and being someone that's experiencing homelessness, there's a lot of risk factors associated with that,” Ingalls said. “I don't want his feet to get infected and then he gets sick and he ends up in the hospital and maybe has more amputations.”
Now that they knew it wasn’t a life-or-death situation, they could pause to provide some comfort and preventative care. It might be one less patient for the health care system on another busy day.

Ingalls, the 24-year-old trainee, eventually plans to go to medical school to become a doctor on the other end of this work. Being a paramedic first means she’ll better understand everything that leads someone to a hospital visit — and all the stresses on this critical system.
Brent Stevenson, deputy chief of operations for Denver Health’s paramedic division, said ambulance services and emergency rooms are prepared to handle the city’s needs. Still, he said if he had a magic wand, he would use it to summon money for more personnel across the system.
“I think we have challenges with growth outpacing resources. And that's not just a Denver Health problem. That's public safety across the board,” he said. “How do we manage our available resources responsibly enough to keep up with that demand?”
Ambulance calls have risen consistently, he said, by about 3 percent each year.

“The impact of 3 percent doesn't seem that great on the surface. But in actuality, as we go, it's the compounded-interest model of how this is going to affect the system,” he told us. “When you're running 130,000 calls and you're looking at a 3 percent increase, it's pretty significant.”
Denver Health is the metro’s main “safety net” hospital, which means it is legally required to help people who can’t pay. The hospital has dealt with surging costs in uncompensated care in recent years, which is why officials asked voters last year to increase sales taxes by a third of a percent to add $70 million annually to its coffers.
Voters approved the measure, and Denver Health recently presented a spending plan for the new fund. The bulk of that money, $36.2 million, will be injected into emergency services like the paramedic division.
‘We don't go into very nice neighborhoods very often.’
It was a typically busy day for Riemer, Ingalls and Fish, which meant lunch continued to elude them.
They picked up a man who had just been rescued from an opioid overdose; his friend had shot naloxone up his nose. The reversal drug put him into an immediate withdrawal, but he was OK. He took a ride to the hospital for a quick check to make sure he was stable, and so he could use the bathroom.
The crew also visited a "regular” in his subsidized apartment downtown — a man with an alcohol dependence who calls 911 once or twice a week. They had seen him just a few days earlier, and noted an empty handle of vodka before they took him outside on a stretcher.
“How much you been drinking, babe?” Riemer asked.

Addiction, homelessness and poverty are symptoms that underpin a lot of calls to paramedics. It’s one reason hospitals like Denver Health have emphasized addressing social determinants of health, things like food access and social support, in an attempt to get ahead of preventable emergencies.
Ingalls said links between economics and health are plainly obvious from her perspective on the job.
“We don't go into very nice neighborhoods very often,” she said. “You're looking at some of our most ill populations.”

Deputy Chief Stevenson and his colleagues keep tabs on the city’s efforts to boost social support. They say new shelters and affordable housing ultimately help people stay healthy, which means they’re less likely to call for an ambulance. They’re also watching federal discussions, particularly over proposed cuts to Medicaid that could strip up to 200,000 Coloradans of health coverage. He said his teams will be even busier if people lose insurance.
“When people don't have access to health care, they revert to 911 and emergency departments as their primary care source, and that's just not sustainable,” Stevenson told us.
Congressional Republicans argue the cuts are about eliminating “waste” and “fraud” in the system. Meanwhile, cities across the nation have long debated whether addiction and visible poverty should be addressed by arresting people, providing more services or some combination.
‘You’re safe’: An assault, and a suicide risk
The team responded to another call Uptown. A man who works in the neighborhood had been hit in the head with a heavy chain and was bleeding from the back of his head. They treated him and gave him a short ride back to his office; then, they saw his assailant scaling a nearby apartment building.

For a moment, it seemed as if the man was about to jump off the roof, but police officers and firefighters coaxed him back down a ladder. They restrained him as they brought him into Riemer’s ambulance. He squirmed and whimpered.
Ingalls was ordered to sedate him. She spoke softly to him as she prepared an IV.
“You’re OK. You’re doing really well,” she said softly. “You’re safe.”

Riemer teaches trainees to be kind to patients, whether they’re on their way to jail or living on a sidewalk.
“One of my biggest pieces of advice is always treat your patients with respect, because we're all one bad choice away from living in the shelter next to these guys,” she said. “Let's be honest, eggs are $10 to a dozen and we're all one bad choice away from it. So treat 'em with respect, treat everybody with dignity and do right by others. You might be roommates with them tomorrow.”
Ingalls said she’s lucky that gentleness comes easy to her. It’s imperative when it comes to treating people in crisis, like someone who’s been handcuffed to a stretcher is being taken away unwillingly.

“Empathy is a very, very large part of our job. It's honestly most of what we do,” she said. “He's a person. He should be treated like a person, and he was scared. So explaining to him that he was safe — he felt like he wanted to hurt himself, but this is a safe place and we're helping.”
It’s one reason Riemer hopes her trainee, Ingalls, doesn’t stay in this job for too long. Many paramedics turn this into a lifelong career, but she said Ingalls’ drive and care should grow beyond an ambulance.
“She's smart enough,” Riemer said. “She should go to med school.”

The job is frenzied and unpredictable, but that’s all in a day’s work
The time for hot dogs came and went as the trio’s shift ended. They still made time for one of Riemer’s traditions, a stop by the 6th Avenue Chipotle for iced tea, which she usually gets free of charge.
Back at headquarters, they cleaned out their ambulance and filled out paperwork on everyone they’d helped. It had been another demanding, 10-hour day. They were used to that — even thrived on it.
“Getting a good save is a really unexplainable feeling that is hard to compare to anything,” Fish said. “Those highs, you can ride for quite some time.”

He added it can be hard to deactivate his paramedic brain when he’s not working. They all perk up when they hear sirens, and they know they need to let themselves rest.
But while Riemer said most of her colleagues work four ten-hour shifts a week, she often books five or six shifts. She loves the work; she also could use the money. Denver Health pays paramedics between $31 and $39 per hour.
“I might be a little crazy,” she said. “No, I’ve got three kids. They're expensive.”

So while the work can be grueling, and while it can be difficult to see people at their lowest every day, the job offers a sense of safety in an ever more expensive city.
“It’s one of the most secure jobs that you could have,” Fish said. “No matter what you do to improve the safety of the streets, people are going to get hurt.”
And sometimes you get hot dogs.
“I'm not sad about it. I'm not hungry. It's only a bonus if you get it,” Riemer said as they called it for the day. “Fish is hungry.”
“I will be eating like a pound of chicken when I get home, but that's just me,” Fish interjected. “I’m kind of sad about the hot dog.”